Find out more about how this website uses cookies to enhance your browsing experience.
Scientific Justification for Laser Therapy
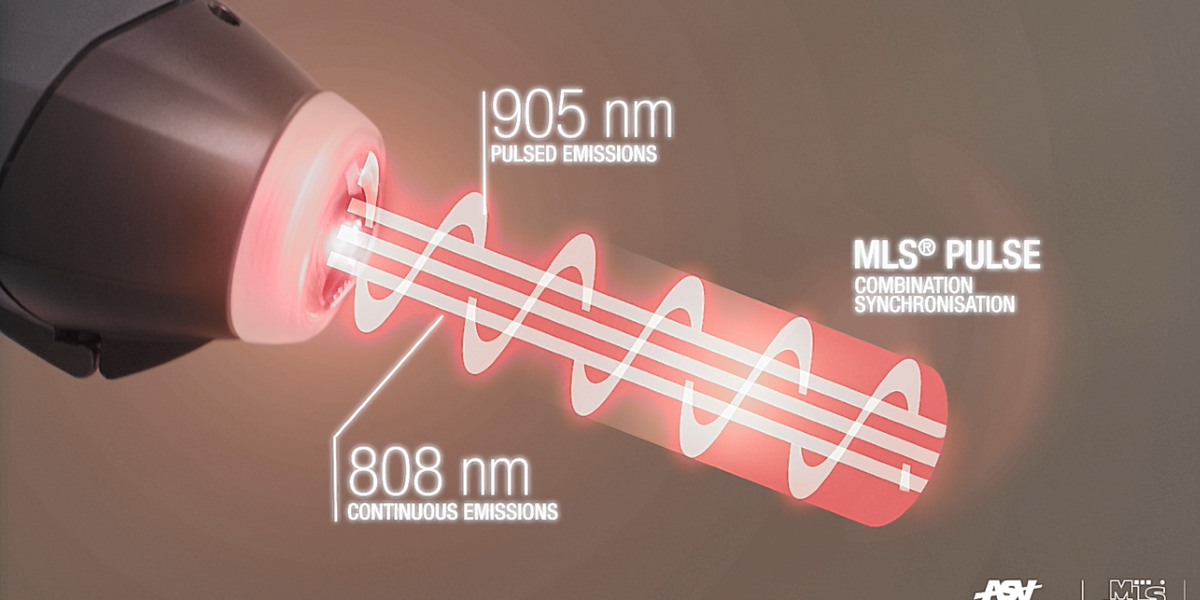
When it comes to chronic pain management, some patients feel like they have tried everything possible. Here comes laser therapy, which provides a non-drug alternative for the management of chronic pain. Celtic SMR is now offering MLS Laser therapy equipment to help healthcare professionals deal with pain, inflammation, oedema and wound healing. Interested in the biochemical mechanism behind the efficacy of Low-Level Laser Therapy (LLLT)? Here is a summary of recent studies on LLLT and its effects at the cellular level.
Pain Relief
Laser Irradiation from LLLT (830nm) induces neural inhibition in peripheral nerves. Photoreceptors in the membranes of mitochondria in axons, absorb laser energy, causing electrochemical changes in the mitochondria. This results in decreased mitochondria membrane permeability (MMP) and lower levels of ATP within neurones. ATP is needed for nerve function including microtubule maintenance and molecular drivers for fast axonal flow. The lower ATP levels slow the speed of neural transmission and the amplitude of the action potential (Chow, David & Armati 2007), resulting in neural inhibition and analgesia.
Trigger points are highly innervated myofascial areas which are often the focus of pain initiated by muscular tension. The muscular tension leads to a cycle of increased pain and further muscular spasm as tissue hypoxia increases. LLLT causes neural inhibition of the peripheral nerves supplying the muscle, immediately reducing pain and muscle spasm. Laser irradiation also energises the surrounding tissue improving microcirculation (photobiomodulation effect), improving oxygen supply to hypoxic tissues and removing waste cellular metabolites (Simunovic 1996). This enables the muscles to relax and movement to be quickly restored.This can be seen clinically, by palpating the trigger point, feeling the spasm and painful reaction of the patient. Apply the MLS laser radiation for 20 secs on pain setting over the trigger point. The muscle will immediately relax in most cases and the pain is significantly diminished.
Anti-inflammatory Effects
Multiple studies have measured the effects of LLLT on inflammatory mediators (Bjordal JM, Lopes-Martins RA, Iversen VV. 2017; Xavier M & al. 2010). In studies, laser irradiation significantly reduces inflammatory cytokines (interleukin-1, interleukin-6, tissue necrosis factor- alpha) thus reducing acute phase protein production and the inflammatory process in the acute and chronic phases. Studies have also found that cyclo-oxygenase (COX-2) mRNA expression in the acute phase is also reduced leading to lower levels of PGF 2-alpha (Albertini R et al. 2007; Kajagar BM et al. 2012).
Anti-oedema Effect
Studies show that LLLT can be effective in reducing tissue oedema (Baxter & al. 2017; Wigg 2009). Laser irradiation stimulates lymph flow, reducing interstitial fluid in the tissue and reducing pro-inflammatory cytokines that cause inflammation and increase oedema. Laser irradiation also energises the surrounding tissue improving microcirculation (photobiomodulation effect), further reducing oedema.
Wound Healing
Laser therapy reduces the inflammatory reaction, induces increased collagen deposition and a greater proliferation of myofibroblasts to speed up healing wound (Medrado & al. 2003).